Humira stopped working for me in January 2013. I started taking Simponi in March and to date no real relief. I had an appointment with my Dermatologist today and she suggested Stelara. I called my Rheumy today and left a message that I wanted to change another TNF or Stelara.
Any feedback from people who are on Stelara for PsA would be appreciated.
I have never tried Stelara. I don't have much P but wicked PsA. I am on my 4 or 5th biologic Remicade. So far so good.
Stelera is still not approved for PsA so unless its prescribed by your dermo, you may not get insurance approval for PsA. In the USA Its is approved for psoriasis. The Phase 3 numbers for PsA we questionable and are under review. I know there were several here that have used it and was just approved in Europe.
I don't have much P either. I want to use Remicade, but the insurance is is making it tough. I'm trying to get J&J to pick up the difference and let me pay my copay.
michael in vermont said:
I have never tried Stelara. I don't have much P but wicked PsA. I am on my 4 or 5th biologic Remicade. So far so good.
She said she would write a script for me. She works closely with my Rheumy and they have two others with PsA on it now with positive results. I see no need to continue with Simponi if I'm not getting anything out of it.
tntlamb said:
Stelera is still not approved for PsA so unless its prescribed by your dermo, you may not get insurance approval for PsA. In the USA Its is approved for psoriasis. The Phase 3 numbers for PsA we questionable and are under review. I know there were several here that have used it and was just approved in Europe.
I'm not disagreeing with trying it. No reason to use a drug that doesn't work (Simponi) getting it by the insurance companies is the secret. If you failed Simponi I sure would be trying something different that remicade.......
I was wondering if anyone has any updates to this? I have been diagnosed with Psa (no P). They tried MTX with no effect. I am now on Stelara. I get my 2nd injection in 3 days. So far, no bad side effects like MTX, but no improvement on the PsA.
I know Stelara has only been approved for PsA in the last few years. Since then, have folks been having success with it? Just curious if this is a good option for PsA, or if other bioligics might be better.
Peace,
-Dave
Hi Dave,
Stelara has been proven quite effective for some PsA sufferers. It really does take quite a while to build up in your body. I took all the loading doses and waited the 3 month period, took that dose and was still waiting to see results. There was a twinge of improvement during the loading doses but, unfortunately, that medicine didn’t do it for me. This, of course, doesn’t mean it isn’t wildly successful for others.
Thankfully there are so many new choices of biological medications around, so my rheumy moved me from Stelara to Cosentyx which seems to be (in an over-cautiously optimistic view and after having gone through the loading and regular doses for two months) beginning to work for me.
Keep talking to your rheumatologist about how you feel, how well you’re able to function (or not), any stiffness or swelling, and how fatigued you are. These are important for you to share with your rhemy so together you can make an informed choice about staying on a medication, adding other DMARDs to the mix, or switching to something else. Fire away with more questions if you have them!
Didn’t work for me, but maybe I didn’t wait long enough.
Hello, i have been taking Stelara successfully for several years now. The psoriasis under my nails cleared up and my chart says “no active psoriatic arthritis”. I still have pain of course. My doc tells me I have a lot of osteoarthritis also and that seems to be advancing. But no swollen joints and no psoriasis patches on skin (however, I did not have skin psoriasis patches before taking Stelara). I did have a recent increase in sed rate of 17 points in recent blood test. But it still is only 5 points above “normal”.
Stelara has been wonderful for me so far. No side effects and the shot doesn’t hurt at all, unless my arthritis in my hands makes me mess up pushing the syringe!
You’re the first person I’ve found who’s on stelara for longer and it actually works… mostly it’s only people who have been on it for max 6 months or who stopped…
I had my second dose the Friday before last… a month after the first… and I do feel a lot better, but no where near good  I’m hopeful it will keep getting better.
I’m hopeful it will keep getting better.
even baby steps are steps in the right direction! Glad you’re starting to feel a little better.
The secret with any of the BIO’s is to build on the baby steps from the meds and take advantage of the small improvements with the PT and flexibility work. The most improvement comes from what you can do for yourself when and as you can all the meds can do is give you some opportunity.
Hey all,
I had my second dose this morning. First time I have ever injected myself with anything. That seemed to go OK, I guess. I certainly forgot the nurse’s recommendation to count to 5 as you push the meds in. It was quick and out. I was really nervous and wanted to get it done with. The one thing I will give it is that it doesn’t knock my on my rear for 3-4 days like those MTX pills did.
Between shot-one and today, I don’t notice any improvements. I have seen this statement a lot here and maybe I too am in denial, but I wonder if I even have PsA. Never had any skin issues, nail issues, etc. Just tendinitis in a few joints (4). And they, apart from one, don’t have any visible inflammation. Just pain that PT can’t get to go away. But, blood work came positive for HLA-B27, so that, I guess, is a check in the “you’ve got it” column.
Lately I’ve been having these all over “body aches” It’s not local to joints, but maybe it’s emanating from my rib cage (doesn’t feel “inside” like heartburn). But these waves come up in the afternoon and it is hard to function or do anything but lay down in a quiet, warm place. I can’t find any other PsA forums where this is described.
I have read a lot (LOT) on PsA and Stelara and I wonder if it is the most effective treatment. It certainly stinks to have to wait 6 months to be able to say whether it works or not. Long time to be on the wrong thing.
Anyways, I will try to post updates. And if others who have been on longer for PsA have stories, I would like to know what I may be in store for.
Peace,
-Dave
Have you talked to your doc about the afternoon episodes? My guess is that being HLA-B27 positive the pain is starting at T-11,12 and radiates to the front which is fairly classic spondylitis something the are saying now happens to about half of us. T-11,12 and L-4,5 pretty much take the brunt of abuse to our back.
That being said the cyclical nature of it concerns me as well. Also not uncommon is SVT from the weakened muscles/tendons around the heart. Sometimes you feel the “palpatations” other time you don’t. In any event you NEED answers.
FWIW “success” with BIOs is pretty sneaky. I didn’t realize my first one was working until one morning my wife got all excited when I tied my own shoes. It wasn’t even something I had thought about. Then I realized there were other equally subtle changes I hadn’t even noticed…
I have an appointment with her Thursday. It is just my 3 mo followup from the last time she saw me, but it does come at a “good” time.
Others here have expressed frustrations with finding a good RA doc, and I seem to be among them. She is very hard to get a hold of. When these aches started, I called. After 5 consecutive days of leaving messages, the nurse finally called me back and said she sent in Tylenol 3’s but didn’t need to see me.
This hasn’t been the first issue. When it took a few weeks to get to her about the problems I was having with MTX. I went to my GP back then, and he referred me to another RA doc. But that one was booked until mid August. I have an appt with him then, but it has meant 2 months (plus one to go) dealing with the current doc.
I don’t know if RA docs just don’t have the ability to deal with people quickly, but my luck so far has not been too good with responsive docs.
In my research, spondylitis was something that came up and is on my laundry list of “could this be me” topics to bring up.
Peace,
-Dave
@dwlemen The diseases have been reclassified FWIW: We all now have Seronegative Spondyloaropathy and there is more to come…
Those break down to: PsA, Ankylosing Spondylitis, Reactive Arthritis, and enteropathic arthritis The whole AS thing got out of hand and it as a diagnoses is pretty much going back to what it used to be which was a severe spinal arthritis that lead to fusion. The newer Rheumies ar now defining things in terms of Axial Spondyloaropathy, Peripheral Spondyloaropathy or some combination. They are even getting away from the word arthritis (thank god)
The name is not near as important as the treatment…
Sounds like costocondritis, which is common, that is enthesis of the joints in the rib cage.
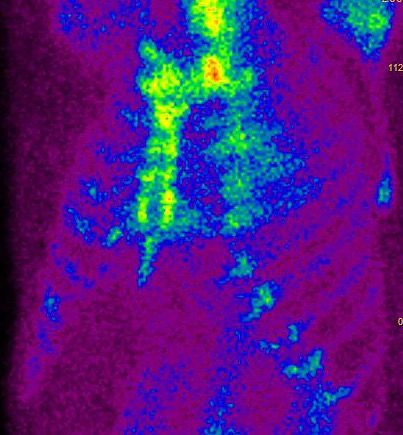
I had a lot of imaging for that, nuclear imaging, and CT.
You should make framed copies of that a sell as limited edition photographs. It beautiful. Not the costo of course that looks ouchy. But the composition is incredible and I don’t like modern art.