New member here. I have a question to put out here. In addition to taking vital signs and med review, it seems to have become routine in the past couple of years for all doctor visits to include the question "Are you in any pain right now?" Since I am always in pain, as are the other people with PSA here, I am curious as to how people answer that question? I have decided to consider my own baseline pain as a new "zero" and then I answer them based on how much worse than baseline I might feel that day, but I always wonder, what other people with chronic pain do. This is not just a rheumatology visit, my PCP, my cardiologist, any visit, anywhere, for any reason, they always ask if I am in pain. So, what do you all do with that question, do you answer truthfully, or do you even take that question seriously?
I answer honestly (sometimes it's a 4, sometimes it's a 7). I follow up saying that I have PsA, I always have pain, and that my disease and pain is treated by my rheumatologist.
That way I get honest info in my chart, BUT I don't come across as 'drug seeking' (ie, getting pain meds from multiple practitioners could red flag me) and I am not putting this particular practitioner in the spot of treating pain from a condition that is not their primary field.
I feel it's really important to be honest with each of my practitioners about how I'm doing. For example, when I'm in a lot of pain my blood pressure can shoot up (mine is usually low) and become high enough for them to be concerned. This is a temporary effect anyone working with me needs to know. The practitioners will see my med list, and KNOW something is going on that is complex. Being honest about my pain helps back that up.
Honesty may not be the best policy with the people you see. It works for me, right now, with the medical practitioners I see.
I have not been asked that, by anyone other than my rheumy. I do know that this is supposed to be routine though. I would answer yes as well, that I have a chronic disease, but that it is not anything that needs to be dealt with at the moment. My rheumy doesn't need to ask that specific question. As she does her exam, we talk about how things are going, and what has been giving me trouble.
In health care, pain is now seen as the "Fifth Vital Sign". That's the "why" behind it, in case anyone was curious. Pain affects other things like BP and HR, so it is important to know. For example: We still haven't figured out if my hypertension is "essential hypertension", related to high NSAID use, or simply a response to pain because all 3 occurred at around the same time. Either way, we are treating it.
My baseline pain is usually a 4-5. I tend to hover there, and I can function there. (Its a fine line though, because for some reason, any increase in pain above that is really hard for me to cope with.) My docs know that's my number and that I have a chronic condition, and like Stoney does, I tell new practitioners that I have an underlying condition. I explain my "baseline" and that I'm okay there. I think it's important to know what a patient's baseline is, so that variations can be investigated.
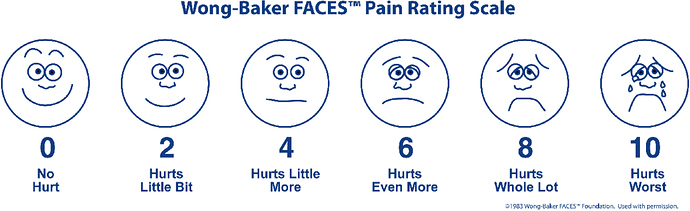
I hate the numeric pain scale with a passion. Patients don't know how to use it, or how to assign a number to their pain, and it's so very subjective. I like the "Wong Baker Faces" scale better. The nurse can show a picture with different faces and different states of pain, then matches the face to a number. I find it much easier to relate to. Here's an image of it:
Such an interesting question/ post. Thanks for sharing it.
My first rheumy's office always asked, via both the form to fill out while sitting in the waiting room and then again by the medical assistant while measuring blood pressure, weight, etc. To my astonishment, the medical assistant always sounded shocked, absolutely shocked when I answered in the affirmative. Seriously? It's a rheumatologist's office! Then they would ask what hurts. Again, they would be incredulous if I mentioned more than one or two areas. The situation does not lend itself to truth-telling.
Like Grumpy Cat, I also hate the numerical scale. I have lived with some amount of pain for almost 30 years now. I do my absolute best to ignore it. The number I come up with is often more about how well I'm ignoring it than a measure of how bad it actually is.
This is an interesting issue for me too especially as I saw in the last letter my rheumy wrote to my GP he quoted my pain assessment and then gave next to it his clinical assessment of my pain level (only 0.5 different, thankfully). Have to say I felt a bit ticked off about this because pain is pain and it's also very subjective because we can never experience someone elses pain the way they do. Like Grumpycat I seem to have a baseline pain level which I can deal with and function at but it doesn't take much of an increase to give me a problem. I'd been thinking about how I could quantify the scale in terms of how pain affects me so I could use that with my docs but now I've seen the 'Wong Baker Faces' this does it for me. Thanks Grumpycat.
I am very fortunate that the faces have been used as an assessment tool for all of the medical facilities that I have been in recently. They are all connected to Providence Medical. (KUDDOS) I still make sure l tell each person involved in my care that I can usually function until the pain makes me dizzy and then I get nausea, between 8 and 10 on the number scale.The tears are usually rolling by themselves by then. I don't even notice if it is too bad because I cannot feel that side of my face nor can I feel my legs and feet much below my knees, apparently . So in this case, the " Wong Baker Faces" make perfect sense. As a professional who used to teach non-verbal communication skills in toddlers and young children I cannot offer a better scale. I used them daily to asses my students everyday needs :)
I have encountered the same thing at the Rheums office-stunned that I have pain. I just take it that lots of people don’t really understand this disease or that most patients are relatively well managed on their meds and that I’m a little atypical. ![]()
Louise said:
My first rheumy’s office always asked, via both the form to fill out while sitting in the waiting room and then again by the medical assistant while measuring blood pressure, weight, etc. To my astonishment, the medical assistant always sounded shocked, absolutely shocked when I answered in the affirmative. Seriously? It’s a rheumatologist’s office! Then they would ask what hurts. Again, they would be incredulous if I mentioned more than one or two areas. The situation does not lend itself to truth-telling.
Like Grumpy Cat, I also hate the numerical scale. I have lived with some amount of pain for almost 30 years now. I do my absolute best to ignore it. The number I come up with is often more about how well I’m ignoring it than a measure of how bad it actually is.
Thank you everyone for your replies. I like the idea of having a short and sweet explanation that I have PSA, that I have chronic pain with that, and that my rheumatologist is dealing with it. It makes perfect sense, but for whatever reason, never occurred to me! :)
And Grumpy Cat - Interesting what you say about your BP. I was also diagnosed with hypertension at the same time that they started to realize I had an autoimmune process going on (last June), and underwent extensive workup to rule out the "scary" reasons for my blood pressure to be so high (ruled out renal artery stenosis, heart failure, etc...). Cardiologist ended up deciding I have "regular high blood pressure" (his words)... but I cannot help question whether it was caused or exacerbated by the systemic inflammation.
I'm also in the same boat with hypertension. First knew I had above normal BP readings was late 2005 but since then inspite of eventual medication it has continued to climb.
Whilst I have a family history of hypertension and other heart disease related issues, I think mine is partly genes, the PsA and the leflunomide. A week ago I was pushing readings of 222/126. My meds have been tweaked and brought it down to 149/101 this morning. The systolic of 149 is about 'normal' for me but the diastolic 101 is still way too high so when I'm back at the docs for my monthly blood test tomorrow I'm going to get my nurse check again with my doc. I don't think they realise (no matter how often I say it) how much this worries me given that both my parents died very young - 43 and 58 years old and I'm now slap bang in the middle at 50!
At least I've now stopped the leflunomide so as this slowly gets out my system I hope it will bring my BP down without having to take too much more medication for it.
So I think that there is definitely a connection with the inflammation of PsA and also potentially the meds used to treat it.
I was almost positive the Hypertension had to have had something to do with this because for my entire life until a few years ago my bp had always been so low I needed to be careful to eat right! Until I was over fifty I ran about 120/60 at every checkup. After I got really ill three years ago my normal ran about 139/85 for the longest time with meds when averaged. However, every night it can and frequently has spiked to 198/101 or even as high as 220 /110. This is alarming to say the least. It does this nearly every night. But under stress, such as Dr appointments and such it usually only rises to about 158/85.
I have been on Lisinopril for three years now and because it averages out it is apparently considered under control. I had times when I was in severe pain and very broken out in plaques that my BP would be high during the day as well, this occurred on especially pustular days.These where also days of very high anxiety due to the intense itching and the burning pain of the rash itself. So... in this case it was most probably caused by the pain, I don't think any of the meds I was on back then where PsA meds.
I have noticed in the last three weeks since they have upped the dosages on the Gabapentin and added the Diclofenac and Topomax my pressure is running at about 190/100 in the a.m when I awake. Definitely a thing to put on my list for check-up discussion next week. My Grams stroked out at eighty five with a BP of !90 /180 !!!! she died of stroke at ninety after years of not knowing who/ where, she /I was and my dad had a massive heart attack at the age of seventy- five for which he received a lovely quadruple bypass and spent the rest of his life regretting his smoking years and his high BP. They both had PsA .
Much research needs to be done. I urge everyone to contribute to that in any way you possibly can whether it be here through Ben's friends and knowledge or donating to your local research hospital or even donating blood at a lab that is doing PsA testing, become a part of global warming research ( yes! our disease is chemically induced and environmentally triggered as well) just do one thing that can help all of us learn and grow and heal.......
Sorry if I offend any one.... this is only my humble opinion and I really care about you guys because you have helped me so I climb on my soap box :[ I hope I did not hijack this thread I don't remember the origianal content .. If I did I apologize
Guys, I am going to start a BP thread. This is interesting and should be discussed further!
crazylady said:
I was almost positive the Hypertension had to have had something to do with this because for my entire life until a few years ago my bp had always been so low I needed to be careful to eat right! Until I was over fifty I ran about 120/60 at every checkup. After I got really ill three years ago my normal ran about 139/85 for the longest time with meds when averaged. However, every night it can and frequently has spiked to 198/101 or even as high as 220 /110. This is alarming to say the least. It does this nearly every night. But under stress, such as Dr appointments and such it usually only rises to about 158/85.
I have been on Lisinopril for three years now and because it averages out it is apparently considered under control. I had times when I was in severe pain and very broken out in plaques that my BP would be high during the day as well, this occurred on especially pustular days.These where also days of very high anxiety due to the intense itching and the burning pain of the rash itself. So… in this case it was most probably caused by the pain, I don’t think any of the meds I was on back then where PsA meds.
I have noticed in the last three weeks since they have upped the dosages on the Gabapentin and added the Diclofenac and Topomax my pressure is running at about 190/100 in the a.m when I awake. Definitely a thing to put on my list for check-up discussion next week. My Grams stroked out at eighty five with a BP of !90 /180 !!! she died of stroke at ninety after years of not knowing who/ where, she /I was and my dad had a massive heart attack at the age of seventy- five for which he received a lovely quadruple bypass and spent the rest of his life regretting his smoking years and his high BP. They both had PsA .
Much research needs to be done. I urge everyone to contribute to that in any way you possibly can whether it be here through Ben’s friends and knowledge or donating to your local research hospital or even donating blood at a lab that is doing PsA testing, become a part of global warming research ( yes! our disease is chemically induced and environmentally triggered as well) just do one thing that can help all of us learn and grow and heal…
Sorry if I offend any one… this is only my humble opinion and I really care about you guys because you have helped me so I climb on my soap box :[ I hope I did not hijack this thread I don’t remember the origianal content … If I did I apologize
I've never seen the Wong-Baker faces. I like those since I always have a hard time rating my pain. I always wonder what I am comparing it to and if I have rated myself correctly. Thanks, GrumpyCat. I, too, have a level of pain that I am always at, but can function. That puts everything into perspective for me.
My rhuemy doesn't ask me that question. What I have learned is that regardless of what he asks me, I need to tell him details on any pain etc. Otherwise he won't get the message on how I am doing.
For me pain is rated on what I can and can't do. I also point out if I have pain in new spots or if I feel it is spreading into another area. For example, from my hands is radiates into the wrists and arms.
All my doctors ask me how much pain I'm in. For many, it's asked regularly because pain can increase your blood pressure, so if my normally LOW blood pressure is around the normal range or slightly above that, they don't freak out if my pain is an 8 or higher. My rheumy not only asks how my pain is, but specifics about my pain.
I do, however, have an issue with standard pain scales. I have been to the ER in pain greater than Wong-Baker can chart. I prefer the Allie Brosh scale: http://rannygahoots.blogspot.com/2013/04/how-do-you-feel-remix.html (scroll down for Allie Brosh from Hyperbole and a Half's pain scale.) ;)
 I wish they had that pain scale in the docs offices. It really is much more accurate.
I wish they had that pain scale in the docs offices. It really is much more accurate.
Hi there Shelly. I get what you mean by viewing your baseline as "0" but if that's what you report to the doctor's office they aren't going to take that very seriously. They do want to know if you're in pain and how bad it is, and reporting it according to their pain scale allows for more accurate documentation. As an example: as a nurse, I've had patients tell me their pain is a level 15. I will remind them that I cannot chart that, I have to use our scale. From http://pain.about.com/od/testingdiagnosis/a/pain_scales.html
"When a nurse asks you to rate your pain, try to be honest. Don’t exaggerate your pain. If you rate your pain as 10 out of 10, but are chatting happily on the phone with your spouse, you are probably not rating it accurately. This is also true if you rate your pain as a two, yet you feel like it might make you faint. The more accurately you describe your pain experience, the better your caregivers can help you control your pain."
Myself, I always feel at a disadvantage when asked the pain question. Often my doctor appointments are in the afternoon-after I've been awake for several hours. By then my pain (if I'm not putting pressure on the sore joints) is around a 5. They miss out getting to see me when I first wake up and can barely open my hands and am shuffling when I walk-when my pain is around a 7-8.
I find it really helps to keep a pain diary of sorts. Help to show any trends or whatnot.
Meanwhile, to end on a laugh, do not underestimate how painful a frozen periogi is when dropped on an inflamed joint. Yowza. I was hopping around the kitchen on foot singing some songs.
Oh,yes, I believe you about the frozen pierogi. Might as well drop a rock on your toe. Ouch!
I understand, I think it is necessary to accurately attest to the pain I am having at the time. I think I have to just think about it ahead of time, and have an answer ready. Usually I am not ready for the question. The pain diary is a good idea too.
I admit to giggling a little when I read this. I was in the ER one time, in incredible amounts of pain, with neck and shoulders so inflamed that I couldn't lift my arms. At all. My husband dropped me off, and the nurse had to enter ALL my information into their new system. She needed my id, my insurance card, my doctors' information ... all of which I needed to fish out of my purse while unable to lift my arms. I found this highly amusing, so was laughing about it. Then I got to triage and the nurse asked me what I was in for, my pain level, etc. I told her she didn't have a number high enough on her pain scale and she looked at me funny and asked why, then, I was laughing. I told her I was in so much pain I had two options, 1. laugh hysterically or 2. cry hysterically, and I thought the ER staff would much more appreciate the former.
Sunny said:
"When a nurse asks you to rate your pain, try to be honest. Don’t exaggerate your pain. If you rate your pain as 10 out of 10, but are chatting happily on the phone with your spouse, you are probably not rating it accurately. This is also true if you rate your pain as a two, yet you feel like it might make you faint. The more accurately you describe your pain experience, the better your caregivers can help you control your pain."
THIS. The more miserable I am the more jokes I make with staff. Most get it, but sometimes I need to explain that I could either be having an epic screaming breakdown at the moment, or letting some of it off with jokes with the people who have to power to help me.
At the rheumy last week I explained that my pain was on par with the last few hours of 17 hours of labor with each of my kids. I explain I didn't scream or freak out during that either, just curled in on myself more and more, and yes, still made a few jokes with the labor nurse.
nym said:
I told her I was in so much pain I had two options, 1. laugh hysterically or 2. cry hysterically, and I thought the ER staff would much more appreciate the former.